This was previously published by the Design for All Institute of India
Steps toward integrative palliative
care in the developing world
Thomas Ask, John Boll, Alexander Nesbitt
Abstract
Treatment for suffering in low resource areas can benefit from easy access to medicines that treat pain, gasping, terminal secretions, nausea, anxiety, and delirium. Because suffering needs to be contextualized within prevailing cultural forces, individuals with communal connections with the patients must be empowered to administer these medications and provide caregiving services.
Additionally, developing low cost
medical dispensing systems allows a wider range of treatment. Artificial intelligence can be coupled to
voice recognition for both patient diagnosis and medical products to improve
efficacy of treatment.
Design can address complex problems through inquiry, synthesis and
creative exploration. Problems that lie
outside mechanistic solutions are fertile areas for design processes that
strive to creatively motivate improvements.
Improving healthcare is a type of problem that challenges deductive
logic and benefits from ‘design thinking’.
This inquiry recognizes the resource driven model of healthcare has
overwhelmed the relational needs required for palliative patient care. This article wishes to extend the medical
discourse beyond the well understood effects of disease and the positivistic
validations of pharmacology. While it is
presumptuous for those steeped in US medical traditions to assert appropriate
systems of palliative care in the developing world, this reflection on
palliative treatment intends to offer a different perspective that appropriate
local decision makers may find helpful.
Palliative care can consider three tracks: medical, relational and
spiritual. The medical realm can include
adjuncts to pharmaceuticals while the relational can cover areas of concern
ranging from the relationship between caregiver and patient to the effect of patient
pain and psychosis on family members. The
spiritual realm addresses deeply held beliefs about the patient’s relationship
to a deity in their faith tradition.
Background
Reducing suffering requires identifying a cultural framework that
connects pain and suffering. The
acceptance of pain and the expectations of palliative care requires a
subjectivist, interpretive epistemology. This epistemology draws upon the
humanist arguments against exclusive positivistic approaches that highlight
limitations of the scientific method and its inappropriateness for assessing
human thought and actions (Feyerabend 1993).
A theoretical
construct for understating the relational component of palliative care, beyond
pharmaceutical approaches, lies with the integration of psychological and
sociological theories. The identity theories, along with the phenomenological
perspective of an ideal self, suggest that when people identify as part of a
group they will deeply nurture each other’s attributes that tend to maintain
the group identity. Motivation for the
cooperative exercise of caretaking can be founded on the development of an
identity associated with a group. The identity theory asserts that one’s self-esteem
is derived from the identity developed from social interactions. The sense of
self is based on the roles that one assumes in a society or group with which
one identifies (West 2014, Stets and
Burke 2000). A shared group identity
can promote a desire to protect against those in other groups.
Pain is shaped by culture into a question
that can be expressed in words, cries, and gestures, which are often recognized
as desperate attempts to share the utter confused loneliness in which pain is
experienced (Illich 1976, p. 140).
Reducing pain and suffering is more
complex than medicinal treatment.
Addressing palliation requires deference to cultural motivators, self-identity
and other powerful, foundational forces.
An effective system for palliative care moves beyond medicine and includes
encouragement of relationally-rooted interaction between the patient and
caregiver as well as spiritual nurturing. The caregiver’s personal connection
with the patient is a key factor in reducing patient anxiety and maintaining
patient dignity. This caregiver relationship
is especially important for terminally ill patients. The medical treatment considers medication appropriate
for treating pain, gasping, terminal secretions, nausea, anxiety, and delirium.
Clinical pain in the developing world
Pain is the most commonly feared symptom
listed by individuals contemplating their eventual terminal illness and death. Unfortunately,
throughout much of the developing world, this fear is realized daily by
hundreds of thousands of people. The World Health Organization estimates that
more than 30 million people each year are in need of care to support them and
palliate their symptoms during their terminal illness, but the vast majority
cannot get this care. Millions suffer from untreated pain annually. This includes more than 5.5 million who die
from cancer and more than one million from end stage AIDS (NGO 2011). Opioids are one essential class of medication
to treat such pain, but access to these medications is very limited in much of
the developing world. Efforts to improve appropriate access to this class of
medications is an important part of the worldwide palliative care movement.
In addition, increasing access to non-opioid medications and non-medication
analgesic measures is also an important component in the effort to reduce
worldwide suffering in the sick and terminally ill.
Comfort kit
In established palliative care systems,
providing patients with an emergency symptom kit (or 'comfort kit') is a
routine component of preparing for the common forms of suffering which afflict
humans contending with advanced illness. The most common such symptoms are
pain, dyspnea (air hunger), nausea and vomiting, delirium (an acute confusional
state) and anxiety. Medications that are commonly included to treat these
symptoms include non-opioid pain medications (such as paracetamol or diclofenac),
anti-anxiety medication (such as lorazepam or diazepam), anti-emetic (vomiting)
medications (such as prochlorperazine), and anti-psychotic medications (such as
haloperidol). Some such packs also include anticholinergic medications to treat
the terminal secretions ('the death rattle') that often accompanies the
terminal state. Provision of a comfort kit including these inexpensive
medications alone, or even better, including simple commonly needed care items
such as simple dressings, a urinal, and perhaps antibiotic ointment, would
greatly enhance the comfort and the dignity for those who are ill and
suffering.
Interpersonal relations
Medical practitioners typically enroll medications to ameliorate acute
symptoms. However, the notion of pain is
contextual and culturally moderated.
Therefore, palliative care must rely most deeply upon the personal
relationship between the caregiver and patient.
The patient must conclude that the caregiver understands the patient’s
suffering. The caregiver must ask the
question, “What would you most like me to know about you so that I can take
care of you?” This inquiry is easy to
present in the abstract but the patient – caregiver relationship is an
entanglement comprised of a web of values, history, social norms, and
regulatory requirements.
A caregiver will never fully understand their patient’s suffering but
must rely upon a deeply held sense of personal responsibility in treating and
comforting the patient. This type of
relationship is more naturally derived from family relationships than from the
medical community. In addition, the patient’s
expectations can motivate the approach to palliation. Consequently, the
attending physician must understand:
- ·
Social and
cultural norms.
- ·
Pain is contextual
and subjective.
- ·
Patient recognizes
not all suffering will be lifted.
- ·
Relationship
between patient and caregivers.
- ·
Effect of illness
on family.
Spiritual
Faith traditions are important in contextualizing suffering and identifying a purpose to pain. Given that the experience of suffering frequently challenges the core of an individual such faith traditions can be an important aspect of providing care both to the patient and their family. Through the values and meaning in a faith tradition suffering can represent a means to develop character and hope in the midst of an illness. Alternatively, patients can believe the purpose of their pain is for discipline or correction or an indiscernible purpose but still governed by their deity. Therefore, addressing the spiritual can be an important part of palliation and subsequent comfort for the suffering individual.
Artificial intelligence (AI) can democratize access to patient
assessment and guide dispensation of medicine.
Computing systems incorporate AI, such as expert systems and artificial
neural networks, that strive to model human thought in a manner that can be
processed on a computer and accessed by a non-expert user. However, sharing human knowledge and
expertise is a difficult task. People
use very sophisticated and intricate thought processes to solve problems, recall
information, and make decisions.
Although expert systems are an excellent technology to save and
disseminate knowledge, transferring that knowledge from the domain expert to
the computer is difficult. Acquiring
knowledge for an expert system is the art of structuring human instincts,
experience, heuristics (“rules of thumb"), guesswork and all the other
words which never can quite explain the human thought process. Expert systems use fuzzy logic to make
decisions. That is, the confidence of an
output is quantified and that value can be handled separately from the
output. The confidence output is then
used in determining the best, final decision of the expert system. The combination of outputs and the confidence
associated with them adds intelligence to the system. In this way the “degree of truth” of
information can be managed.
Neural networks use a large number of processors with each
artificial neuron dedicated to a specific task.
The neural networks organize the links between inputs, outputs and
hidden intermediate layers of decision making.
Sensory or database information is fed through this network with each
neuron processing the data independently and progressing its results through
the network. Generally, a feed forward
approach is used where information flows from the input neurons, through the
intermediate neurons and finally to the output without a feedback mechanism. In this manner, large amounts of information are
processed to identify relationships and therefore create a dynamic algorithm
that can accurately develop conclusions from salient inputs.
Voice recognition is often coupled with AI allowing computing systems
to recognize natural language usage and discern emotion. AI driven voice recognition allows simplified
access to computing power. Currently
voice systems are more than 97 percent accurate in identifying individual words
and are being quickly implemented due to commercial interests (Brown 2016).
However, reliance upon AI driven voice recognition has potential
problems with error and abuse.
Systemic approaches
Improving the quality of life for people contending with the symptoms of
serious illness requires the care best offered through those who have a
personal connection to the patient. Medical
approaches typically involve a professional caregiving team who develop and
execute a plan of care (Ferris 2002). However, where
this resource intensive approach is not possible, a system of palliative care
requires altruistic volunteers to provide treatment and personal support for the
patient. These volunteers are educated and authorized to give support, evaluate
and treat using prescribed protocols.
The volunteers are given comfort kits through the medical
establishment. If a volunteer from a
family, community, or religious group is unable to provide care, a
paraprofessional would need to be engaged; however, this is not the optimal
arrangement because the altruism becomes distorted by financial forces.
The comfort kit would need to be issued specifically for one patient;
however, the comfort kits have value and therefore present potential for
misuse. The contents could be resold,
which is the most direct problem with the effective distribution of comfort kits. In addition to financial gain, the
distribution system provides power over the patient that could be misused. Additionally, administration of medicine could
be met by resistance within the medical establishment as well as social forces that
resist a lay person’s ability to dispense medicine. Control of medicine delivery could be
addressed by technical solutions such as time release containers, drone
deliveries or other ‘just in time’ systems.
However, these delivery systems are vulnerable to theft and abuse.
Caregiver training and adjuncts can improve suitability of
treatment. The caregiver adjuncts can
range from video supervision by a physician to cards with photographs and
corresponding treatment protocols. The
medical community must recognize untreated, acute pain can develop into chronic
pain. Therefore, aggressive treatment of
acute pain through opioid and other medicines is recommended so that chronic
pain will be reduced.
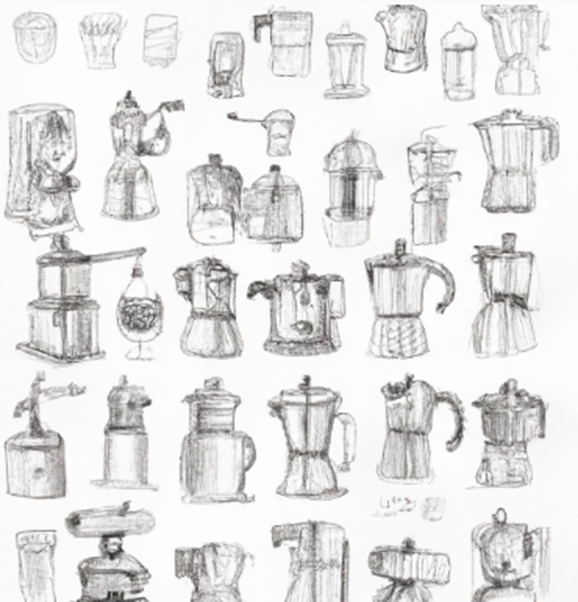
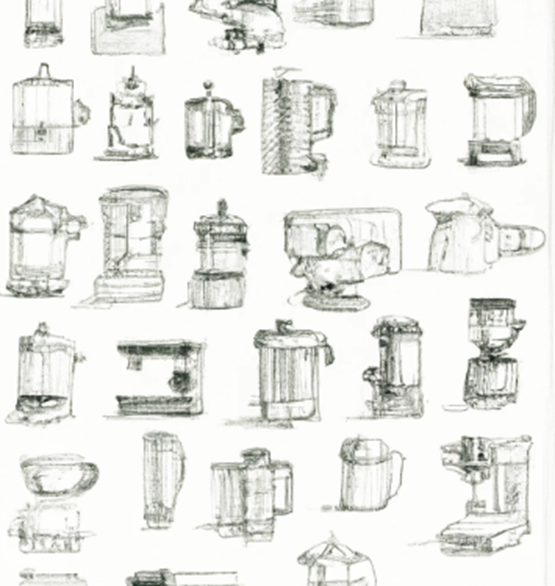
Future approaches
While relationships and spiritual connections will always be key
components of palliative care, mechanistic designs can provide helpful
improvements. These can range from AI
guided medicine dispensing systems to human powered refrigeration
compressors. In addition to AI guided
and remotely based medical supervision, advanced design approaches would call
for low cost/high impact devices. Some
technologies are seemingly difficult to develop such as systems that deter
opiate abuses and secure medicine distribution.
Improvements can be more product specific, such as refrigeration and fluid delivery systems. If patients have refrigeration available they can store and dispense a broader range of medications Appropriate technologies may include human powered refrigeration compressors, solid state thermoelectric refrigeration, high thermal mass systems, and minimized volume super-insulated storage systems. Low cost, easy to use fluid and drug delivery systems such as infusional subcutaneous and syringe driver systems would also aid treatment. Usage of medical products can be facilitated using AI driven voice recognition. Additionally, drone delivered medicine and radio and video communication allows treatment in remote areas.
Conclusion
Palliative care transcends medicine and technology. The spiritual and interpersonal relationships
infuse into patient care in forms that are difficult to characterize. However, in low resource or remote
populations the administration of medicine and care is best administered by
altruistic individuals such as those affiliated with the patient by family,
community or religion. These caregivers
need to be richly empowered to provide treatment necessary to address issues of
pain, dyspnea, nausea and
vomiting, delirium, and anxiety.
Comfort kits should be provided to these
caregivers that would include non-opiate pain killers such as paracetamol and
diclofenac. Other medications would
include paracetamol, diclofenac, lorazepam, diazepam, prochlorperazine, and
haloperidol. Other items such as
bandaging and a urinal would also be provided.
Within the realm of product and
systems designs, technical advances that allow remote monitoring and AI
guidance can provide improved diagnosis and treatment. Moreover, low cost versions of refrigeration
and drug delivery systems will aid in treatment options. Developing non-addictive pain medicines have
been largely unsuccessful; however, customizing pharmaceuticals such as abuse
deterrent opiates designed to genomically key to the individual could reduce
abuse.
Palliative care in the developing
world can be improved by empowering nonmedical personnel who are communally
connected with the patient. These
individuals can best answer the question, “What would you most like me to know about you so that I can take care
of you?”
References
Brown, A. (2016), Talk to Me. American Society of Mechanical Engineers (ASME)
Mechanical Engineering, No. 11, 138, Nov. 2016, pp. 32-37.
Ferris
FD, Balfour HM, Bowen K, Farley J, Hardwick M, Lamontagne C, Lundy M, Syme A,
West P. (2002), A Model to Guide Hospice
Palliative Care. Ottawa, ON: Canadian Hospice Palliative Care Association.
Feyerabend, P. (1993), Against Method.
New York: Verso.
Illich, I. (1976), Medical Nemesis: The expropriation of health. Bantam Books/Random
House.
NGO Human Rights
Watch, (2011) [Online] Global State of
Pain Treatment-Access to Medicines and Palliative Care.
Stets, J. & Burke, P. (2000), Identity Theory and Social Identity Theory.
Social Psychology Quarterly 63,
2.
West, R. (2014), “Communities of innovation: Individual, group, and organizational characteristics leading to greater potential for innovation: A 2013 AECT Research & Theory Division Invited Paper.” TechTrends 58.5, (9), pp. 53-61.